

今天的文献速递内容主要有:
1.吡非尼酮对下降的肺功能和生存的影响。
2.食管癌切除术后的再入院率在区域中心医院和普通医院相似。
3.接受新辅助化疗或放化疗的食管癌患者术后健康相关生活质量下降。
1.
Effect of pirfenidone on lung function decline and survival: 5-yr experience from a real-life IPF cohort from the Czech EMPIRE registry
吡非尼酮对下降的肺功能和生存的影响
INTRODUCTION
Pirfenidone, an antifibrotic drug, slows-down the disease progression in idiopathic pulmonary fibrosis (IPF) over 12 months, however limited data on the decline of lung function and overall survival (OS) in real-world cohorts on longer follow-up exists.
PATIENTS/METHODS
Of the enrolled Czech IPF patients (n = 841) from an EMPIRE registry, 383 (45.5%) received pirfenidone, 218 (25.9%) no-antifibrotic treatment and 240 (28.5%) were excluded (missing data, nintedanib treatment). The 2- and 5-yrs OS and forced vital capacity (FVC) and diffusing lung capacity for carbon monoxide (DLCO) were investigated at treatment initiation and 6, 12, 18 and 24 months’follow-up.
RESULTS
During a 2-yr follow-up, less than a quarter of the patients progressed on pirfenidone as assessed by the decline of >/=10% FVC (17.0%) and >/= 15% DLCO (14.3%). On pirfenidone, the DLCO (>/=10%) declines at 6, 12, 18 and 24 months’ and DLCO (>/=15%) declines at 6, 18 and 24 months’ follow-up were associated with increased mortality. The DLCO decline showed higher predictive value for mortality than FVC decline. In patients with no-antifibrotics, FVC and DLCO declines were not predictive for mortality. Pirfenidone increased 5-yrs OS over no-antifibrotic treatment (55.9% vs 31.5% alive, P = 0.002).
CONCLUSION
Our study observed the 2-yrs sustained effect of pirfenidone on the decline of lung function and survival in the real-world patient’s IPF cohort. DLCO decline of >/=10% shows a potential as a mortality predictor in IPF patients on pirfenidone, and should be routinely evaluated during follow-up examinations.


Journal Respir Res
IF 3.829
摘要要点
介绍 吡非尼酮是一种抗纤维化药物,可在12个月内减缓特发性肺纤维化(idiopathic pulmonary fibrosis, IPF)的进展,但由于随访时间较长,缺乏肺功能和总生存期(overall survival, OS)的相关研究。
方法 该研究共纳入841名IPF患者,其中383(45.5%)名患者接受了吡非尼酮治疗,218(25.9%)名患者未进行抗纤维化治疗,而另外240(28.5%)名患者被排除(数据缺失,尼达尼布治疗)。在治疗开始以及6、12、18和24个月的随访中调查了2年和5年的OS、最大肺活量(forced vital capacity, FVC)以及肺CO弥散能力(DLCO)。
结果 在为期2年的随访中,FVC下降≥10%(17.0%)和DLCO下降≥15%(14.3%)的患者之间,使用吡非尼酮的不到25%。对于使用吡非尼酮的患者,随访6、12、18和24个月时DLCO下降≥10%,以及随访6、18和24个月时DLCO下降≥15%均与死亡率增加相关。与FVC下降相比,DLCO下降的死亡率预测价值更高。对于未使用抗纤维化治疗的患者,FVC和DLCO下降都不能预测死亡率。使用吡非尼酮可提高5年OS(55.9% vs 31.5%)。
结论 该研究发现IPF患者中,持续使用2年吡非尼酮对下降的肺功能和生存有一定影响。吡非尼酮治疗的IPF患者中,DLCO下降≥10%可作为死亡率预测指标,因此应在随访检查中常规评估这项指标。
DOI 10.1186/s12931-019-0977-2
2.
Readmission rates following esophageal cancer resection are similar at regionalized and non-regionalized centers: A population-based cohort study
糖尿病增加食道癌与食管胃交界处癌发病风险
OBJECTIVE
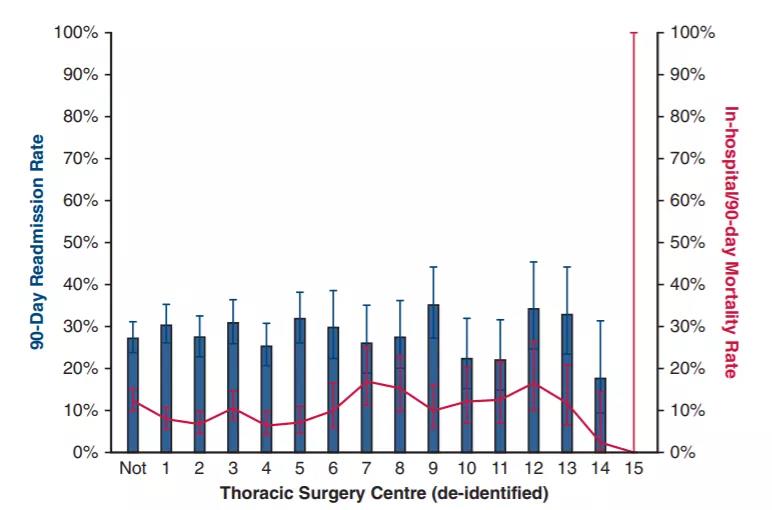
Readmission following esophagectomy affects the patient experience, has important economic implications, and can be tied to hospital reimbursement. Ontario has regionalized thoracic centers; regionalized surgery may lower the readmission rate. We investigated whether surgery at regionalized thoracic centers is associated with reduced readmission following esophageal cancer resection.
METHODS
A retrospective, population-based cohort study (2002-2014) was conducted in Ontario, Canada (population 13.6 million). Adults with resected esophageal cancer were identified through the Ontario Cancer Registry. Multivariable regression was used to estimate the effect of surgery at a regionalized thoracic surgery center on readmission to any Ontario hospital within 90 days following discharge.
RESULTS
Of 3670 patients, 27.9% were readmitted within 90 days of discharge (n = 1022). Median hospital length of stay was 12 days (interquartile range 9-20). The readmission rate at thoracic centers was similar to other hospitals (28.1% vs 27.1%, P = .57). The readmission rate did not change during the 13-year study period. Case-mix adjusted readmission rates varied from 17.6% to 35.2% even across thoracic centers and were not related to hospital volume or perioperative mortality. After adjusting for confounders, we found that surgery at a thoracic center was not significantly associated with readmission (odds ratio, 1.10; 95% confidence interval, 0.95-1.27, P = .22).
CONCLUSIONS
Surgery at a designated thoracic surgery center did not reduce the risk of 90-day readmission following esophageal cancer resection, and readmission rates varied significantly even across thoracic centers. Our results suggest that despite universal, regionalized esophageal cancer care, there appears to be a minimum readmission threshold following esophagectomy that may be clinically necessary.
Journal J Thorac Cardiovasc Surg
IF 5.261
摘要要点
目的 食管切除术后再入院会影响患者的生活质量,具有重要的经济学意义。作者调查了在区域性胸科中心进行食管癌手术是否能降低再入院率。
方法 作者纳入加拿大安大略省接受食管癌手术的3670名患者。分析在区域性胸科中心进行食管癌手术出院后90天内再入院的规律。
结果 1022(27.9%)名患者在出院90天内再入院,住院时间中位数为12天。胸科中心的再入院率与其他医院相似(28.1% vs 27.1%)。所研究的13年数据中,再入院率没有明显变化。整个胸科中心根据病例混杂进行校正后的再入院率从17.6%至35.2%不等,并且与医院规模或围手术期死亡率无关。作者表示在胸科中心进行手术与再入院率没有明显关联(优势比 1.10)。
结论 在指定的胸科中心进行手术并不能降低食道癌切除2后90天再入院风险,即使对于整个胸科中心而言,再入院率也存在明显差异。作者表明,尽管患者接受了普及的区域中心医院的治疗,但是食管切除术后似乎存在最低的再入院阈值,这在临床上可能难以避免。
DOI 10.1016/j.jtcvs.2019.04.061
3.
Health-related quality of life in a randomized trial of neoadjuvant chemotherapy or chemoradiotherapy plus surgery in patients with oesophageal cancer (NeoRes trial)
接受新辅助化疗或放化疗的食管癌患者术后健康相关生活质量下降
BACKGROUND
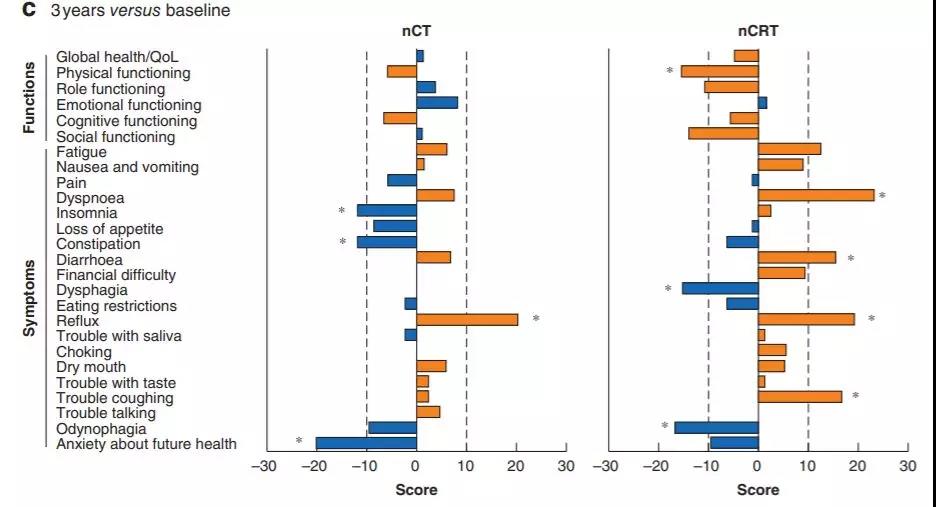
There are few data comparing health-related quality of life (HRQoL) after neoadjuvant chemotherapy alone (nCT) compared with neoadjuvant chemoradiotherapy (nCRT) in patients with oesophageal cancer.
METHODS
In the NeoRes trial, patients were assigned randomly in a 1 : 1 ratio to receive either cisplatin 100 mg/m(2) on day 1 and an infusion of 750 mg per m(2) 5-fluorouracil over 24 h on days 1-5 in three 21-day cycles (nCT) or the same chemotherapy regimen, but with the addition of 40 Gy radiotherapy (nCRT). HRQoL data were collected at baseline, after neoadjuvant therapy and at 1, 3 and 5 years after surgery. The European Organisation for Research and Treatment of Cancer (EORTC) core questionnaire QLQ-C30 and disease-specific modules were used.
RESULTS
Of 181 patients randomized, 165 were included in the analysis of HRQoL. In a direct comparison between the allocated treatments, odynophagia after completion of neoadjuvant therapy but before surgery (P = 0.047) and troublesome coughing at 3 years’ follow-up (P = 0.011) were more pronounced in the nCRT arm. In the longitudinal analyses within each treatment arm, a large deterioration in HRQoL was noted at 1 year. Some recovery was seen in both arms over time but, after 3 and 5 years, patients in the nCRT arm reported more symptoms compared with baseline than patients in the nCT arm.
CONCLUSION
HRQoL after multimodal treatment for cancer of the oesophagus or gastro-oesophageal junction was impaired and more pronounced in patients who underwent nCRT, with only partial recovery over time.
Journal Br J Surg
IF 5.586
摘要要点
背景 关于接受手术治疗的食管癌患者中新辅助化疗(neoadjuvant chemotherapy, nCT)与新辅助放化疗(neoadjuvant chemoradiotherapy, nCRT)后健康相关生活质量(health-related quality of life, HRQoL)的研究十分匮乏。
方法 在NeoRes试验中,患者随机平均分为nCT和nCRT两组,nCT组在第1天接受100 mg / m2顺铂治疗,并在第1-5天的24小时内进行750 mg/m25-氟尿嘧啶注射治疗,持续3个21天化疗周期。nCRT组在相同的化疗方案基础上增加40 Gy放疗。在基线时、新辅助治疗后以及术后1、3和5年收集HRQoL数据。
结果 181例患者中,有165例患者被纳入HRQoL分析。研究发现nCRT组在手术前新辅助治疗后出现吞咽困难,并且在3年的随访中出现影响生活的咳嗽症状。每个治疗组均在术后1年时出现HRQoL大幅度下降。随着时间推移,两组患者都有一定程度的恢复。但是比基线患者相比,术后3年和5年时nCRT组患者的不良症状多于nCT组。
结论 对食道或胃-食道交界处癌症患者进行多方案联合治疗后,HRQoL受到较多不良影响,接受nCRT的患者HRQoL下降更为明显,随着时间推移只有部分改善。
DOI 10.1002/bjs.11246